Metoprolol has been used for high blood pressure and other heart conditions for over 40 years. Some doctors also prescribe it for migraine prevention and abnormal heart rates. This drug is not effective in all patients, and it can cause side effects like low heart rate and loss of libido. Read on to learn more about the uses, side effects, and dosage of metoprolol.
Disclaimer: This post is not a recommendation or endorsement for metoprolol. This medication is FDA-approved for the treatment of specific medical disorders, and can only be taken by prescription and with oversight from a licensed medical professional. We have written this post for informational purposes only, and our goal is to inform people about the science behind metoprolol’s effects, mechanisms, and current medical uses.
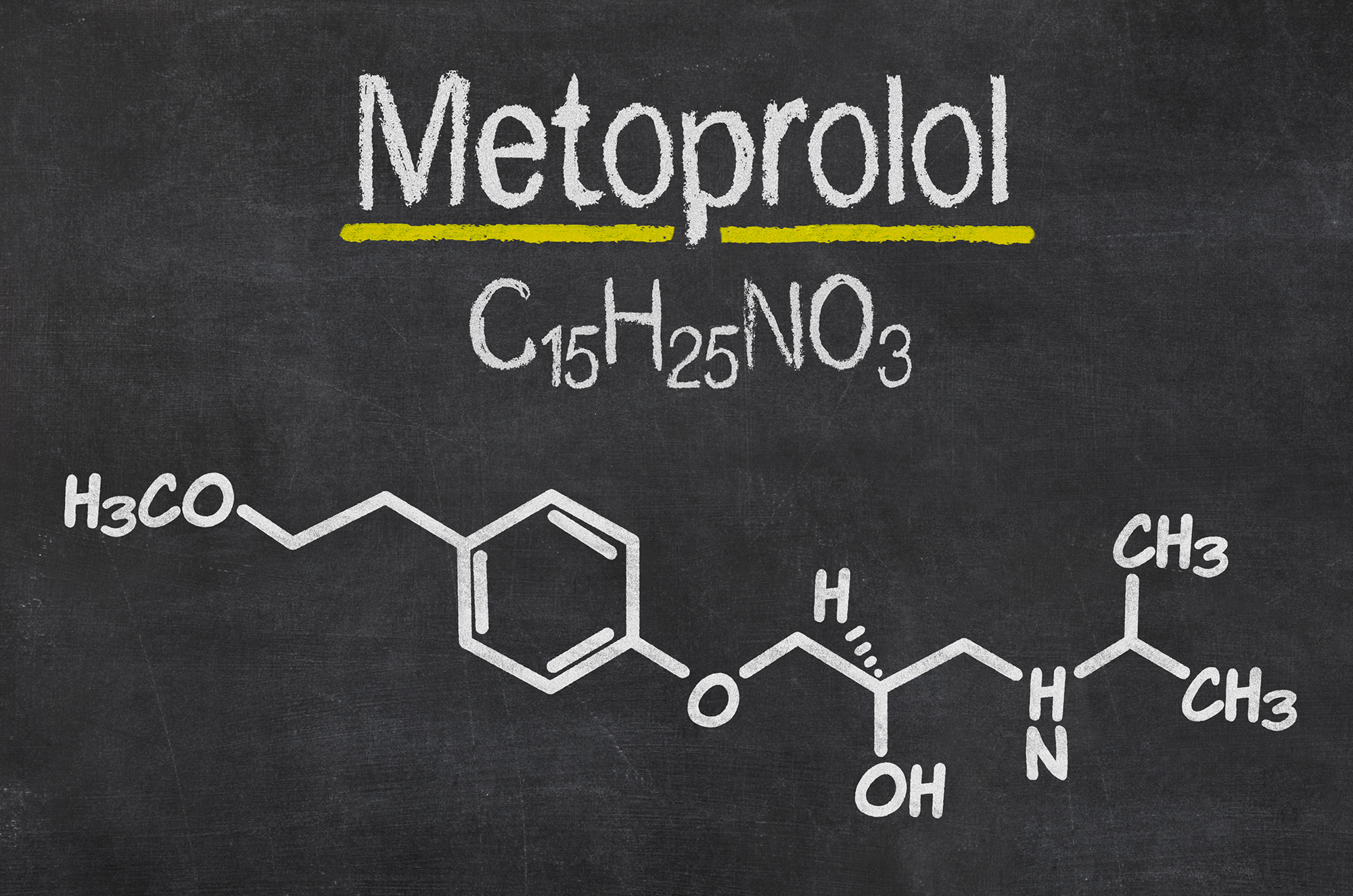
What is Metoprolol?
Metoprolol has been used to treat high blood pressure since 1975. It comes in two forms:
- Immediate release, also known as metoprolol tartrate or the brand name Lopressor
- Extended release, also known as metoprolol succinate or the brand name Toprol XL.
Both types of metoprolol belong to a group of drugs called beta blockers [1, 2].
The major difference between metoprolol tartrate and succinate is what they are used to treat and how frequently they are dosed.
Both can be used to treat high blood pressure and angina (chest pain). Metoprolol tartrate is the only form used to treat myocardial infarction (heart attack), unstable angina, and arrhythmias, while metoprolol succinate is the only form used to treat heart failure.
Other beta blockers include atenolol, bisoprolol, carvedilol, and nebivolol. Although similar to metoprolol, these drugs have some differences in their use and side effects [1, 3].
Mechanism of Action
Beta-blockers are named for their main mechanism of action, which is to block adrenaline receptors, located in the heart and brain [4, 1].
There are multiple types of adrenaline receptors. At normal doses, metoprolol blocks only one type, beta-1 adrenaline receptors. Activated beta-1 receptors raise blood pressure and heart rate, and increase the stress response [5, 6].
Metoprolol achieves its effects by preventing the activation of these receptors.
Metoprolol may reduce heart damage after heart surgery, heart attack, and heart failure. Typically, the heart responds by “remodeling” the injured heart tissue in ways that increase the risk of future heart problems. Metoprolol may reduce these remodeling processes by [7, 8]:
Metoprolol may also reduce inflammation and oxidation in the heart by:
- Lowering levels of the pro-inflammatory cytokines (IL-1β, CXCL1, and TNF-alpha). It also increased the anti-inflammatory cytokine IL-10 (in rats) [11, 12]
- Preventing neutrophils from moving to the heart [13]
- Lowering activity of NF-κB and vascular endothelial growth factor (VEGF), pro-inflammatory chemicals [9, 7]
- Reducing the number of macrophages in arterial plaques (in mice) [12]
- Increasing the number of glucocorticoid receptors, which respond to cortisol [14]
Approved Medical Uses
1) High Blood Pressure
A study of 195 patients with high blood pressure found that both forms of metoprolol reduced blood pressure and heart rate better than placebo following 6 weeks of treatment [15].
In a study of 100 patients with high blood pressure, both forms of metoprolol reduced blood pressure in 93% of patients after 8 weeks [16].
Metoprolol also improved heart function in elderly patients with high blood pressure and heart failure after 3 months of treatment, in a study of 330 people [7].
2) Stable and Unstable Angina (Chest Pain)
Both metoprolol tartrate and succinate are effective at treating stable angina, however, only the tartrate form is used to treat unstable angina [17].
Metoprolol improves angina by reducing “ischemic load” on the heart. This is achieved by through the slowing of the heart rate in patients taking the medication [18].
Metoprolol also helps with exercised induced angina. Often doses are adjusted to an optimal level to help the patient both at rest and during exercise [18].
3) Heart Failure
Note: All metoprolol in the section is referring the succinate form.
In a study of 3991 patients with congestive heart failure, patients given metoprolol had higher chances of survival than the patients given placebo, after 1 year of treatment [19].
In another study of 383 patients with dilated cardiomyopathy, a major cause of heart failure, people treated with metoprolol reported increased levels of life satisfaction and physical activity after 18 months, compared to those given placebo [20].
Metoprolol may provide similar benefits for children with genetic heart conditions. A study of 30 children with heart failure due to inherited heart defects found that metoprolol improved heart function after 3 months of treatment [21].
Despite these positive studies, metoprolol is not considered first line for the treatment of heart failure. Another beta-blocker, carvedilol is superior to metoprolol in the treatment of chronic heart failure [22].
4) Heart Attack Prevention and Recovery
Note: All metoprolol in the section is referring the tartrate form.
A large meta-analysis with a total of over 61,000 patients that experienced a heart attack found that metoprolol reduced the chance of experiencing a second heart attack, but did not reduce the risk of death or of being rehospitalized [22].
Individual studies do suggest that metoprolol may reduce the risk of death following a heart attack. A study of 1,395 patients given metoprolol or placebo after a heart attack found that metoprolol reduced the rate of death by 36%. It also reduced rapid heartbeat (ventricular fibrillation) and prevented further heart attacks in the first 3 months of treatment [23].
After a heart attack, an implant called a stent is sometimes placed in blood vessels of the heart to reopen them. In one study of 270 patients, those who were given metoprolol within 6 hours of a heart attack and who then received a stent had less heart tissue death 1 week after the procedure [24].
Another study of 638 patients with heart stents failed to show a reduction in heart tissue death in patients given metoprolol [25].
In a study of 8,351 people undergoing non-heart surgeries, patients that received metoprolol succinate (extended-release) before surgery who continued taking the drug for a month after surgery had a lower risk of having a heart attack than patients given a placebo. However, the risk of stroke and/or death was increased in the group given metoprolol [26].
Another study followed 599 patients undergoing blood vessel surgery and found that there was no difference in rates of heart attack, risk of dying, or of stroke between the group given metoprolol and the placebo group [27].
Off-Label Uses
Occasionally, doctors will prescribe drugs like metoprolol to help treat conditions that fall outside of the official uses approved by the FDA – also known as “off-label” drug use. Usually, this is done because there is decent evidence that the drug may help, although not enough to get full FDA approval [28].
5) Arrhythmias (Impaired Heartbeat)
Note: All metoprolol in the section is referring the tartrate form.
A study of 20 patients with sinus tachycardia, a form of arrhythmia that causes excessive heart rate, found that metoprolol reduced resting heart rate from 114 to 93 beats per minute after 4 weeks. It also reduced heart rate during daily activity [29].
Metoprolol may not be effective in treating the inherited form of long-QT syndrome, however. A study of 382 people with this form of the syndrome found that metoprolol is not as effective as 2 other beta-blockers (propranolol and nadolol) at preventing the recurrence of symptoms [30].
A pilot study of 215 patients found those that received metoprolol after heart surgery had a lower rate of dangerous arrhythmias (atrial fibrillation) than those given placebo [31].
Rats were given metoprolol after a severe heart attack had lower rates of several types of arrhythmias (including ventricular fibrillation, ventricular tachycardias, and premature ventricular contractions) than rats given a placebo [32].
Long-QT syndrome is a type of arrhythmia that is inherited genetically or caused by lifestyle factors like medications. In mice, metoprolol reduced the symptoms of long-QT syndrome caused by ziprasidone, an antipsychotic medication, and by amitriptyline, an antidepressant [33, 34].
6) Migraine Prevention
A meta-analysis of 4 studies found that metoprolol succinate (extended-release) is more effective in preventing migraine headaches than placebo. Overall, metoprolol reduced the frequency of migraines by approximately 50% [35].
Metoprolol was recommended for the prevention of migraines in a report by the American Academy of Neurology and the American Headache Society [36].
Other Potential Uses
Metoprolol has also been studied for other health conditions. However, keep in mind that the evidence supporting these potential applications is still preliminary, and a lot more research will be needed before they are approved. Therefore, the information below with a grain of salt.
7) Narrowed Heart Valves
Mitral valve stenosis is a narrowing of the heart’s mitral valve, which can block blood flow.
Two studies of mitral valve stenosis, one with 97 participants and another with 34, compared the effects of the drugs metoprolol and ivabradine. The study found that both drugs could reduce resting heart rate, and rate during exercise after 6 weeks of treatment [37, 38].
Metoprolol may also help in the treatment of aortic stenosis. One study of 40 people with asymptomatic aortic stenosis found that the muscles of the heart consumed less oxygen and operated more efficiently after taking metoprolol for 22 weeks [39].
8) Fainting
A study of 54 people showed that metoprolol tartrate (immediate-release) prevented the recurrence of syncope (fainting) over one year of treatment [40].
Metoprolol may also be effective in treating loss of consciousness in children. In a study of 28 children, metoprolol worked as well as the conventional treatments (midodrine and fludrocortisone) in preventing loss of consciousness over a year-long treatment period [41].
9) Traumatic Brain Injury
One study compared the outcomes of 356 patients with traumatic brain injury admitted to the hospital over a 7-year period. Those patients given metoprolol after their injury had a lower risk of death than those who did not receive metoprolol [42].
10) Raynaud’s Syndrome
Raynaud’s syndrome causes narrowing of the small blood vessels (usually in fingers and toes), leading to poor circulation.
One study of 46 patients with both hypertension and Raynaud’s syndrome found that metoprolol combined with felodipine (a calcium channel blocker) improved blood circulation to the fingers and toes [43].
11) Coronary Angiography
Metoprolol is often given to patients before an angiogram to achieve a low enough heart rate for the procedure. A study of 1,871 patients given metoprolol before having a coronary angiogram found that only 1 patient had a negative side effect due to metoprolol (temporary loss of consciousness) [44].
Another study of 662 patients that underwent coronary angiography found no evidence of adverse side effects in any of the cases where patients were given metoprolol to lower heart rate [45].
12) Chagas Disease
Chagas disease, caused by the parasite T. cruzi, can cause heart failure, altered heart rate, sudden death (cardiac arrest), and stroke [46].
In a study of 9 patients, metoprolol reduced symptoms of congestive heart failure due to Chagas disease, including rapid heartbeat and reduced pumping volume, after 10 weeks of treatment [47].
Metoprolol also reduced abnormal heart activity due to Chagas disease in rats [48].
Limitations and Caveats
The effectiveness of metoprolol can vary widely and may be based on a person’s genetic makeup. African-American patients, in particular, are less likely to respond to treatment with metoprolol for heart conditions [49, 50].
Many of the uses of metoprolol have only been studied in a small number of patients, including its potential benefits for vasovagal syncope (fainting), Raynaud’s syndrome, and Chagas disease. Larger studies are needed to confirm the effects of metoprolol on these conditions [40, 47, 43, 51].
Safety & Side Effects
Metoprolol is generally safe at prescribed doses, but can be toxic and even fatal at high doses [52, 53, 54].
There is also a possibility of serious complications and withdrawal symptoms if metoprolol is stopped rapidly [55, 56, 57].
The most commonly reported side effects include:
- Difficulty sleeping [58]
- Erectile dysfunction (in men) [59, 60, 61, 62]
- Sexual dysfunction (in women) [63, 64]
- Abnormally slow heart rate (bradycardia) [65]
Other potential side effects of metoprolol are:
- Increased insulin resistance (in people with diabetes) [66, 67]
- Increase in symptoms of depression and burnout (in people with previously diagnosed psychological disorders) [68]
- Increased triglyceride levels [69]
- Psychosis or delirium, especially in older patients [70, 71]
- Psoriasis [72, 73]
- Sleepwalking [74, 75]
- Hallucinations and vivid dreams [76]
- Lichenoid dermatitis [77]
- Erythema multiforme [78]
Pregnancy and Lactation
Metoprolol should be taken with caution during pregnancy. It does not appear to present a large risk during pregnancy, but it can have effects on newborn infants, including low blood sugar and slowed heartbeat [79].
Pregnancy can change the way the body breaks down metoprolol. Late in pregnancy, women may break down metoprolol more quickly, becoming less responsive to the drug [80].
It is likely safe to breastfeed while taking metoprolol at low doses [81].
Contraindications
Metoprolol must not be used in the presence of the following conditions [82]:
- Uncompensated (advanced) heart failure
- Sick sinus syndrome
- Second or third-degree heart block (in the absence of pacemaker)
- Severely low blood pressure and heart rate (hypotension and bradycardia)
- Hypersensitivity (allergy) to metoprolol
Drug Interactions
Some medications prevent cytochrome P450-2D6, the enzyme that breaks down metoprolol, from functioning properly. This can result in abnormally high levels of metoprolol in the body, which may be toxic. Medications with a confirmed interaction of this type include:
- Vorinostat (suberoylanilide hydroxamic acid), used to treat cutaneous T-cell lymphoma [83]
- Imatinib, which treats various types of cancer [84]
- Paroxetine, fluoxetine, and bupropion, all used as antidepressants [85, 86, 87]
- Mirabegron, which treats overactive bladder [88]
- Ellagic acid and gallic acid, antioxidant supplements [89]
- Terbinafine, which treats fungal infections [90]
Other medications reduce the ability of the gut to absorb metoprolol. These include [91]:
- Diphenhydramine (antihistamine, found in Benadryl)
- Procainamide and quinidine (medications for heart arrhythmia)
- Bisoprolol (treats high blood pressure or heart failure)
Metoprolol may lower the amount of metformin (a medication given for type 2 diabetes and for polycystic ovary syndrome) in the blood. Taking metoprolol and metformin may also result in higher levels of uric acid, which is associated with kidney damage [92, 93].
When used together, metoprolol and angiotensin-converting enzyme inhibitors, commonly used to treat hypertension or heart failure, may increase allergic reactions [94].
Metoprolol vs. Other Drugs
Bisoprolol
A study of 183 patients found that bisoprolol was more effective than metoprolol in reducing heart rate, but the 2 drugs were similar in their ability to reduce blood pressure [95].
Nebivolol
A study of 60 people with mild high blood pressure compared the effects of metoprolol and nebivolol and determined that metoprolol and nebivolol had similar effects. Both reduced blood pressure during exercise and while resting, after 8 weeks of treatment [96].
Nebivolol may be more effective at reducing oxidative stress than metoprolol [97].
Carvedilol
Metoprolol and carvedilol were compared in a study of 3,029 patients, which showed that carvedilol was better than metoprolol at preventing death in people with chronic heart failure over 5 years. These findings have been questioned, however, because of the doses and form of metoprolol used. Thus, more research is needed to confirm these results [98].
Combinations With Other Drugs
Metoprolol may also be used in combination with other medication to lower blood pressure. One of 1,092 patients showed that a combination of metoprolol and felodipine lowered blood pressure more effectively than either drug alone after 9 weeks, but at lower doses and with fewer side effects [99, 100].
In a study of 403 participants, a combination of amlodipine and metoprolol reduced blood pressure more effectively than either medication alone, following 8 weeks of treatment [101].
Dosage
When taken as a pill to treat high blood pressure, 100 to 200 mg of metoprolol succinate is standard once a day in an extended-release form, or patients may take 50 to 100 mg twice a day of instant-release metoprolol tartrate [16, 102, 103, 104, 105].
While 100 to 200 mg is also used for cardioprotection after heart attacks and heart failure, some patients respond to low doses, such as less than 100 mg [106, 107].
Genetics
Please keep in mind that the research in this field is still young. Make sure to consult your doctor, and don’t make any changes to your treatment based on the studies described below.
Metoprolol is only effective in treating high blood pressure in about 50 to 60% of people. Genetic differences in patients are the main reasons that some people respond to metoprolol while others do not. Although several genes accounting for this have been found, much of this variation in responsiveness has not yet been explained [108, 109].
CYP2D6
Cytochrome P450 2D6 (CYP2D6) is the enzyme that breaks down metoprolol in the body. This gene has many different forms in humans that result in metoprolol being either quickly broken down and removed from the blood or being broken down more slowly. The fast-acting forms metabolize up to 36x more metoprolol than the slower forms [110, 111, 112].
People who break metoprolol down slowly, due to their slow-acting version of the CYP2D6 enzyme, are more likely to respond to metoprolol treatment. They show larger reductions in blood pressure and heart rate than people who break down metoprolol quickly [113, 114].
β-Adrenaline Receptors
Metoprolol functions by activating type 1 beta adrenaline receptors. People with a certain form of the type 1 beta adrenaline receptor gene may need lower doses of metoprolol to lower blood pressure. A study of 29 men taking metoprolol showed that men with this form of the gene had lower levels of active renin, an enzyme produced by the kidneys that reduce blood pressure [115].
The amount of type 1 beta adrenaline receptors that a person produces, a type of epigenetic modification, could also affect how a person responds to metoprolol [108, 116].
Angiotensin-converting enzyme
The angiotensin-converting enzyme produces angiotensin II, a molecule that activates the “fight or flight” response activity. Metoprolol works in part by reducing levels of angiotensin II [117].
Multiple forms of the gene coding for this enzyme exist in humans, and this may impact how a person reacts to metoprolol. One form of the gene results in lower angiotensin II levels. People with this version had a larger decrease in heart rate after taking metoprolol for 8 weeks, in a study of 96 Han Chinese patients with high blood pressure [117].


