I’ve been getting more and more people with outstanding infections. Helping people who have chronic infections can be tricky because they are most likely to react to supplements, which is why such people often require a ‘slower’ approach (one that lessens reactions).
Identifying infections can also be really tricky. Is it bacterial, fungal, parasitic or viral? Biofilms make the equation more complex because even if someone took an anti-microbial that would kill their infection, biofilms can prevent this from happening.
What Are Biofilms?
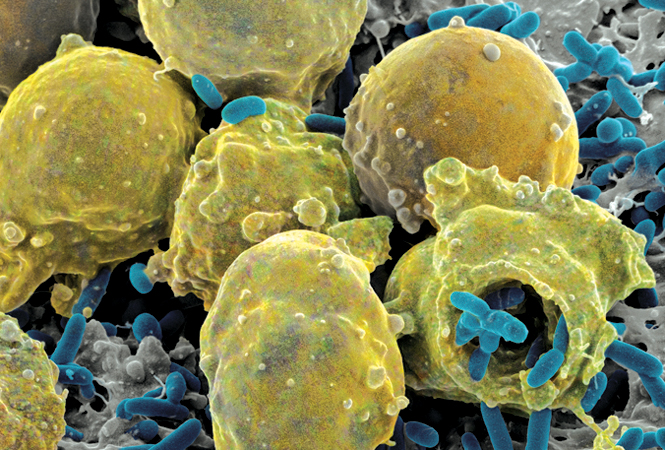
Biofilm formation occurs when free-floating microorganisms attach themselves to a surface and create a colony [1].
They secrete materials (extracellular polymers) that provide a structural matrix that adheres to surfaces [1].
Biofilms and Infection
About 80% of human infections affecting the gut, mouth, sex organs, lungs, heart, teeth, eyes, ear, and skin are caused by biofilm-associated microorganisms [2].
Some scientists think that antibiotics can actually induce biofilm formation [3].
Biofilms may be a reason why some people suddenly do worse for no apparent reason – because after biofilms grow, they disperse.
Biofilms also might be a reason why people avoid herbal supplements.
For example, if you take a supplement that breaks up biofilms, some of the bacterial products can be released, which can cause an immune reaction.
Why Are Biofilms Bad?
Currently, there is a large sum of money and research aimed at the use of and protection against biofilms [1].
Biofilms Are Resistant to Antibiotics:
Because biofilms protect the bacteria, infections are often more resistant to traditional antimicrobial treatments, making them a serious health risk [1].
Most, if not all, antibiotics and antiseptics fail to eradicate mature biofilms, and today, the poor efficiency of available antibiotics is a major challenge for the successful treatment of chronic infections [4].
Biofilm bacteria generally tolerate antibiotic treatment and this is because antibiotics can’t pass through the biofilm enough [3, 5].
Biofilms are known to be involved in many chronic infections such as in a chronic wound, lung, ear, heart and nose infections [4].
Most people (59%) with chronic sinus infections were found to have a bacterial biofilm, whereas none of the controls (people who didn’t have a sinus infection) had bacterial biofilm [6].
The most common biofilm that you might be familiar with is the plaque in your teeth [4].
Current Methods of Treatment:
At present, the most efficient treatment for biofilm infection is to mechanically remove the infected area or body part. This is sometimes possible if the focus is a catheter, an implant, or an infected organ that is eligible for transplantation [4].
So far, the two main strategies for preventing or suppressing bacterial biofilm infections are (1) early aggressive antibiotic treatment before the biofilm is formed or (2) chronic suppressive antibiotic treatment when the biofilm is established if it cannot be removed physically [4].
There are more than one million cases of catheter-associated urinary tract infections reported each year, many of which can be attributed to biofilm-associated bacteria [1].
Catheters have a surface that is conducive for biofilms to form, which is why infections are so common.
In the body, when biofilms form, they form a protective layer by which bacteria evade the immune system and antimicrobials.
Bacteria become tolerant to antibiotics and most other antimicrobial agents [4].
So if you have a fungal or bacterial infection that’s coated with a biofilm, one theory suggests that normal antibiotics and antifungals won’t kill the infection. This theory hasn’t been proven, though.
If you have a bacterial infection that persists despite antibiotic therapy and you have a high level of proinflammatory cytokines, some scientists think this implies that you either have a biofilm or a nonbacterial infection [4].
Factors that Inhibit Biofilms: Natural Biofilm Disruptors
When bacteria form biofilms, they don’t lump together by chance.
In order to form biofilms, bacteria need to communicate with each other [7].
One way to disrupt biofilm formation is to interrupt bacterial communication, also known as quorum sensing (QS) [7].
Scientists hypothesize that Quorum Sensing Inhibitors interrupt bacterial communication signals, which prevent them from aggregating [7].
If you think you have an infection, it’s important to urgently speak to a doctor to get an adequate diagnosis and treatment. You may try the additional strategies listed below if you and your doctor determine that they could be appropriate. None of these strategies should ever be done in place of what your doctor recommends or prescribes.
Also, have in mind that supplements have not been approved by the FDA for medical use. In general, dietary supplements lack solid clinical research. Regulations set manufacturing standards for supplements but don’t guarantee that they’re safe or effective. Speak with your doctor before supplementing.
Foods
- Linoleic acid (omega-6) [8, 9]
- Oleic Acid/Olive Oil [8]
- Honey [10]
- Propolis (candida biofilm) [11]
- Apple Cider Vinegar [12] -physiologically tolerable concentrations of acetic acid can completely eradicate bacteria in mature biofilms vitro.
- Caprylic acid (G+,-, fungal) [13]
- Stevia [14]
- Xylitol [15]
- Garlic [16, 17]
- Manuka [18]
- Ginger [19] (G+,-)
- Cranberry [20]
Non-Herbal Biofilm Disruptors
- Ozone [21, 22]
- Chitosan [23, 24, 9]
- NAC [25]
- Lactoferrin [15, 26]
- EDTA [27] – EDTA likely exerts antimicrobial activity by chelating magnesium and calcium – minerals necessary for growth and membrane stability and may also display anti-biofilm activity by reducing biofilm material (EPS) production and/or enhancing the detachment of bacterial cells from the biofilm. Magnesium, calcium, iron, zinc, and manganese appear to stabilize the biofilm matrix of a variety of organisms by enhancing structural integrity through electrostatic interactions that serve to cross-link the matrix [5].
- Zinc [28]
- Iron (29)
- Manganese [5]
- High alkalinity (magnesium?) [30]
- Monolaurin [31] (G+)
- Colloidal Silver [32]
- Zeolite (Acidithiobacillus thiooxidans) [33]
- L Reuteri [34]
- Citrate? [35] – Calcium Citrate, Magnesium Citrate
- Norspermidine (found in chlorella) [3]
Enzymes
- Trypsin [36]
- Serratiopeptidase [37]
- Nattokinase [38]
Herbal Biofilm Disruptors
- Andrographis [39]
- Curcumin [40, 9]
- Berberine [41, 9]
- Cinnamon/Cinnamaldehyde [42, 43] and Cinnamon essential oil [43]
- Black cumin oil/Thymoquinone [44]
- Boswellia [45]
- Vanilla
- Ginkgo
- Oregano Oil (carvacrol+thymol) [46]
- Quercetin [47]
- Apigenin [48]
- Naringenin [48]
- St John’s Wort [49]
- Kaempferol [48]
- Rosmarinic acid (higher concentrations) [50]
- Baicalein [31]
- Neem [11, 51]
- Gentian violet [52]
- Mangosteen (streptococcus) [53]
- Alfalfa [54]
- Eugenol [42, 9, 43] – found in Tulsi, clove essential oil and cinnamon essential oil

