White blood cells are immune cells that help fight infections and diseases. Read on to learn what high or low white blood cell counts could mean.
What Are White Blood Cells?
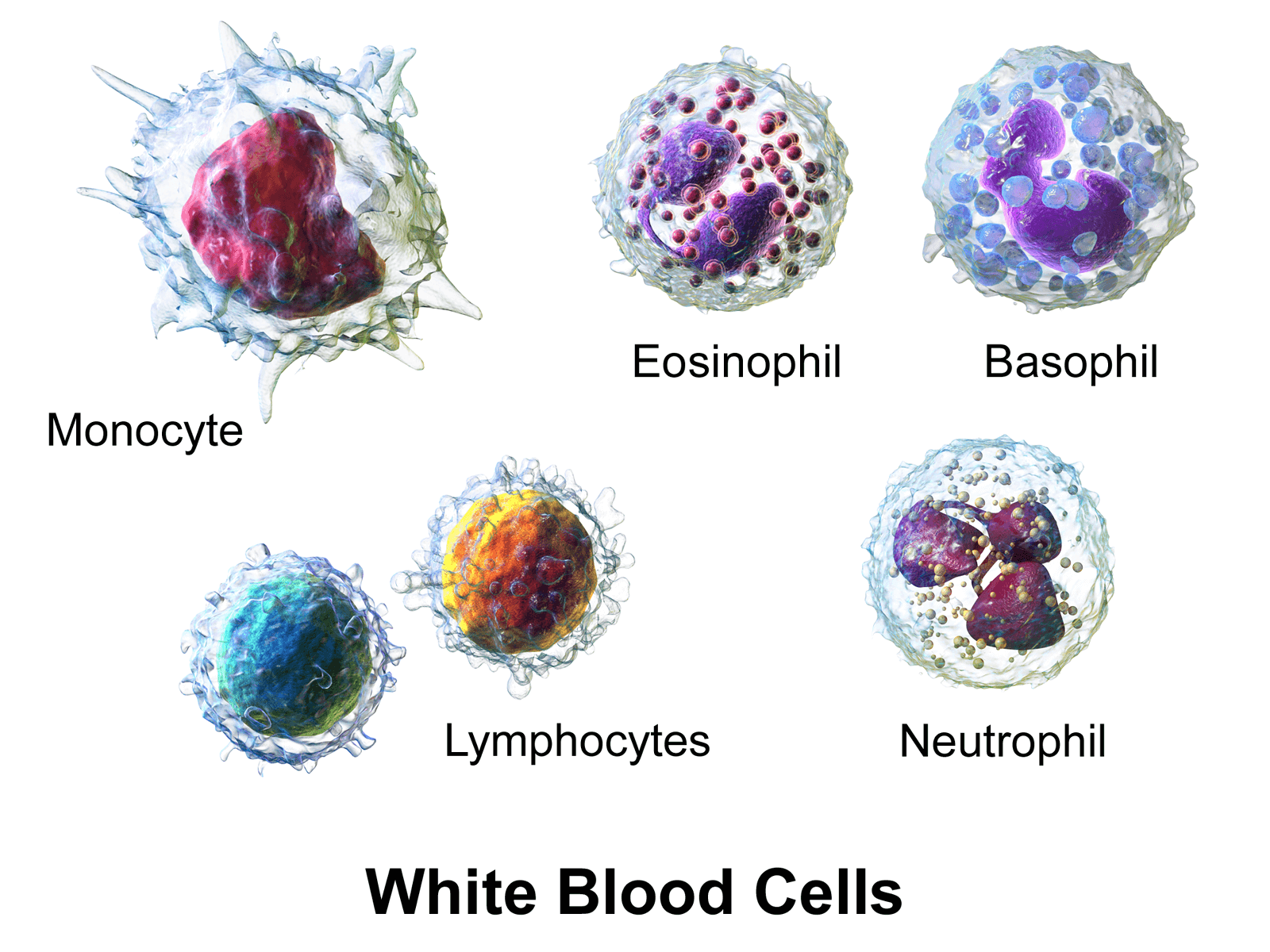
White blood cells, or leukocytes, help the body fight infection. The five types of white blood cells are basophils, neutrophils, eosinophils, lymphocytes, and monocytes [1].
There are associations between white blood cell (WBC) count and the proteins in red blood cells, heart rate, weight, cholesterol, uric acid, creatinine, sex, ethnic origin, blood pressure, height, and blood sugar in both men and women [2].
Having a high level of white blood cells is bad, but for some people having too low of a level means that they won’t be able to effectively fight infections.
Why Are Low Levels of White Blood Cells Bad?
Your doctor will interpret your WBC test results, taking into account your medical history and other tests results. A result that is slightly high may not be of medical significance, as this test often varies from day to day and from person to person.
Having too low of a white blood cell count can be a sign of an immune system that is not capable of handling infections properly.
Also, low white blood cells tend to indicate other issues in the body. For example, in some autoimmune conditions, white blood cells can be lower. If you are worried about a low WBC count, work with your doctor to determine and address the underlying causes and develop an appropriate treatment plan.
A low white blood cell count can be caused by the following (not an exhaustive list):
- Infections, including viral infections (especially HIV/AIDS)
- Chronic inflammation, which can use up white blood cells faster than they are produced
- Certain disorders present at birth that involve diminished bone marrow function
- Cancer or other diseases that damage bone marrow, such as leukemia; also, chemotherapy or radiation therapy
- Drugs, such as antibiotics, which destroy white blood cells
- Autoimmune disorders such as sarcoidosis, lupus, rheumatoid arthritis
- Nutrient deficiencies
The causes listed here are commonly associated with this symptom, but low WBCs are not enough to identify the underlying condition responsible. Work with your doctor or other health care professional for an accurate diagnosis.
Why Are High Levels of White Blood Cells Bad?
Your doctor will interpret your WBC test results, taking into account your medical history and other tests results. A result that is slightly high may not be of medical significance, as this test often varies from day to day and from person to person.
If you are worried about a high WBC count, work with your doctor to determine and address the underlying causes and develop an appropriate treatment plan.
White blood cells are immune cells capable of causing oxidative stress and damage.
Leukocytes participate in the inflammation process, are recruited at the site of endothelial injury, and form foam cells in the plaque [3].
Interleukins and tumor necrosis factor-α are released from activated leukocytes and can cause endothelial dysfunction [3].
White blood cells can build up in the arteries and cause hardening, contributing to plaques and potentially heart attacks. Besides hardening of the arteries, high levels of white blood cells can cause problems with circulation, blood thickening, and increased release of proinflammatory cytokines.
The following is a list of links to conditions or diseases that are exacerbated by high levels of white blood cells:
1) Mortality
Repeatedly, studies have shown that WBC is a clinical marker of inflammation and a strong predictor of the risk of dying (mortality) from all causes [4, 5].
The total WBC count is an independent predictor of mortality in older adults, but the monocyte subtype provides greater predictability [6].
2) Heart Disease
WBC counts were almost linearly associated with cardiovascular mortality [4].
WBC counts within 24 hours of hospital admission for a heart attack is a strong and independent predictor of in-hospital and 30-day mortality risk. Relative to those patients in the lowest 20%, patients in the highest 20% of WBC counts were 3 times more likely to die at 30 days [7].
Circulating WBCs amplifies oxidative stress in heart failure [8].
3) Cancer
A high WBC count was also significantly associated with cancer-related mortality [9].
4) Diabetes
A high WBC value predicted diabetes when adjusted for age, sex, body fat, and other established predictors of diabetes [10].
Also, a high WBC count at baseline was associated with a subsequent worsening of insulin resistance and the development of type 2 diabetes in Pima Indians [10].
These findings are consistent with the hypothesis that chronic activation of the immune system may play a role in causing type 2 diabetes [10].
5) Dialysis
An increased neutrophil count and reduced lymphocyte count are independent predictors of increased mortality risk in dialysis patients [11].
Factors that Increase White Blood Cell Levels
If you have low white blood cell levels, the first thing to do is to work with your doctor to address any underlying causes. You may try the additional strategies listed below if you and your doctor determine that they could be appropriate. None of these strategies should ever be done in place of what your doctor recommends or prescribes!
Lifestyle Interventions
1) Consult Your Doctor
Low WBCs often indicate an underlying health problem that must be addressed, and your doctor is the best resource to figure out the appropriate treatment and management strategies. You and your doctor may discuss medications, supplements, or alternative treatments like acupuncture or sauna bathing, depending on what’s causing your WBCs to be low.
Meanwhile, if you think your immune system may be compromised, take extra precautions with your hygiene. Make sure you wash your hands and avoid contact with people who may be sick.
2) Heavy Resistance Exercise
During and after exercise in weight training males, WBC increased. This shows that leukocyte counts can significantly increase in response to heavy-resistance training/exercise [12].
During the recovery phase after submaximal exercise, there was an increase in the numbers of total leukocytes, neutrophils, lymphocytes, and monocytes [13].
Be cautious with exercise, particularly if your low WBC count is caused by an underlying illness. Your doctor can help you determine if your body can handle this kind of stress.
Nutritional Factors
3) Healthy Diet
A healthy diet rich in fruits and vegetables can help balance your immune system and maintain optimal health. Fruits and vegetables contain important vitamins, minerals, and polyphenols.
Some foods and nutrients have been specifically found to increase WBC count in animal models. These include:
- Vitamin B12 helps to increase WBC counts. However, this effect was only seen in rats with protein deficiency; rats who ate a normal level of protein had unchanged WBC counts [14].
- Garlic, which slightly increased total WBC in rats [15].
- Noni juice, which increased WBC and other blood and platelets counts in rats [16].
- Fish oil, which increased WBCs in broiler chickens [17].
4) Folate
Folate deficiency is associated with decreases in lymphocytes and granulocytes, two types of white blood cells [18].
In a randomized clinical trial (RCT), folic acid supplementation increased WBC counts in children receiving the anti-seizure medication carbamazepine [19].
5) Shark Liver Oil
Shark liver oil has a lot of alkylglycerols, which are fats that stimulate the production of WBCs. Shark liver oil supplementation was shown to increase WBC counts in humans [20].
Substances and Pathways That Increase WBC Levels
These are the natural regulatory pathways that normally stimulate white blood cells in your body. While they are associated with increased WBCs, there is little evidence that attempting to modulate them will affect your immune system in any significant or beneficial way.
Talk to your doctor about the most appropriate strategies to treat underlying conditions and manage your white blood cell count.
1) Cortisol/Glucocorticoids
Glucocorticoids/cortisol can increase the number of WBCs in the body [21].
Glucocorticoids (includes cortisol) increase leukocytes/WBCs in blood but decrease the number of lymphocytes, eosinophils, monocytes, and basophils [21].
A single dose of cortisol resulted in a 70% decrease in lymphocytes and a 90% decrease in monocytes, occurring 4 to 6 hours after treatment and persisting for about 24 hours. Cell numbers then rise 24 to 72 hours after treatment [21].
We strongly recommend against using cortisol to increase WBCs. It is always preferable to talk to your doctor about strategies to treat underlying conditions causing abnormal WBCs.
2) Leptin
WBCs are correlated to the amount of body fat in humans.
Leptin stimulates myeloid production, which is a precursor of WBCs [22].
Leptin is a hormone found in fat cells. The amount that circulates in humans is in direct proportion to the percentage of body fat. Leptin and the leptin receptor work together to stimulate blood cell production [23].
In Pima Indians, the WBC count is positively correlated with the percentage of body fat. The more fat the subjects had, the more WBCs they had in their bodies [23].
Weight loss can reduce the WBC count [24].
After controlling for age and gender, percent body fat accounted for 23% of the variance in the WBC count [23].
3) Adrenaline and Noradrenaline
Adrenaline and noradrenaline were infused into 5 healthy subjects. Total WBC counts increased in response to adrenaline and noradrenaline. Both alpha- and beta-adrenergic receptors are involved in the mobilization of lymphocytes [25].
4) MSH
MSH is capable of increasing WBCs in diabetic rats, who had lower levels [26].
5) Thyroid Hormones
Thyroid hormones may slightly increase WBCs. People who are hypothyroid have slightly lower WBC counts and it increases when they normalize their levels [27].
6) IGF-1
IGF-I stimulates a rapid increase in a number of immune cells, including WBCs, and helps increase the overall effectiveness of the immune system [28].
IGF-1 has an antiapoptotic (inhibits cell death) effect on WBC count and may increase their number [29].
7) Growth Hormone
Growth hormone, like IGF-I, also stimulates a rapid increase in a number of immune cells, including WBCs, and helps increase the overall effectiveness of the immune system [28].
Growth hormone alone (administered via injection to rats) increased WBC count. This was due to an increase in the number of lymphocytes and monocytes [30].
8) Prolactin
Prolactin has a variety of immune-stimulating effects [28].
Injection of prolactin in mice increases WBCs [31].
Prolactin goes up after people have a seizure – and so do WBCs (but the authors didn’t connect the two) [32].
9) Insulin
The WBC count is related to blood insulin levels and insulin resistance in healthy individuals of Pima Indian descent. Higher insulin levels correlated to higher WBC counts [33].
However, this could simply be because WBCs increase insulin resistance, and insulin levels are higher in insulin-resistant states [34].
Using liver and fat cells from mice and humans as well as live mouse models, scientists discovered that an enzyme secreted by neutrophils called neutrophil elastase (NE) impaired insulin signaling and boosted resistance. Conversely, deletion of NE in obese mice fed a high-fat diet improved insulin sensitivity [34].
Factors that Decrease White Blood Cell Levels
Work with your doctor to treat any underlying conditions causing unusual WBC levels. You may try the additional strategies listed below if you and your doctor determine that they could be appropriate. None of these strategies should ever be done in place of what your doctor recommends or prescribes!
Lifestyle Choices
1) Reduce Stress
Stress can increase cortisol, adrenaline, and prolactin, all of which can increase WBCs. Reducing stress can decrease these hormones and help normalize high WBC counts [35, 36].
2) Improve Sleep Quality
Interrupted or poor quality sleep can increase the markers of inflammation, including white blood cell count. Make sure to get enough sleep at around the same time each night to help keep inflammation down [37, 38].
3) Stop Smoking
WBCs in male smokers were significantly higher than in ex-smokers and non-smokers. In current cigarette smokers, WBCs were related to the number of cigarettes smoked, the amount of inhalation, and the duration of smoking [39].
Obviously, smoking is not recommended as a means to increase WBCs. If you smoke, we recommend talking to your doctor about strategies to quit.
4) Reduce Simple Carbs
High carb meals are capable of increasing leptin, insulin and IGF-1, more so than by consuming fat. The high-carb “Western diet” has also been associated with increased WBC count and increased inflammation. Reducing carbs in your diet may help bring down elevated WBCs, reduce inflammation, and possibly prevent insulin resistance [40, 41, 42, 43].
5) Reduce Calories
Restricting calories in the long term has been linked to lower WBC counts without harmful effects to the immune system. In a two-year study of 218 healthy adults, the calorie-restricted adults, those who restricted calories also experienced a 0.6 unit reduction in WBCs. The effect of caloric restriction on people with elevated initial WBC counts is unknown [44].
Substances and Pathways
These are the natural substances and pathways that normally regulate white blood cells in your body. While they are associated with increased WBCs, there is little evidence that attempting to modulate them will affect your immune system in any significant or beneficial way.
Talk to your doctor about the most appropriate strategies to treat underlying conditions and manage your white blood cell count. None of these strategies should be used to replace your doctor’s recommendations!
1) Zinc
Zinc plays an important role in immune function. Zinc deficiency increased the number of total WBCs, granulocytes (neutrophil, eosinophil, and basophil), and monocytes in mice without changing the number of lymphocytes [45].
Zinc deficiency induces the overall stress response which may result in increased WBCs [46].
Therefore, supplementation with zinc (if you’re deficient) may help decrease high WBCs.
2) Selenium
WBCs decreased in men who ate a high-selenium diet. The decrease may have been due to changes in granulocytes [47].
Optimal Reference Range for White Blood Cells
Lab results are commonly shown as a set of values known as a reference range, which is sometimes referred to as a “normal range.” A reference range includes upper and lower limits of a lab test based on a group of otherwise healthy people.
Your healthcare provider will compare your lab test results with reference values to see if any of your results fall outside the range of expected values. By doing so, you and your healthcare provider can gain clues to help identify possible conditions or diseases.
Participants in a prospective cohort study with baseline WBC < 3,500 and WBCs > 6,000 had higher mortality than those in the 3,500 to 6,000 (WBC/mm^3) range [4].
In an additional independent study that covered 7 countries, results concluded that each point increase in WBCs was associated with 21% higher 5-year heart disease mortality (after adjustment for risk factors) [48].
A WBC count between 3.5 (3,500) and 6.0 (6,000) is considered normal.
WBC counts of 9,000 to 10,000 showed a 3.2 fold increase for the risk of cardiovascular disease mortality compared to those with WBC counts of 4,000 to 4,900 [5].
WBCs can vary from person to person based on a multitude of factors.

